Latest News & Promos
- Details
- Written by The Community Eyecare Team

It is safe to say that many people prefer shopping online to shopping in stores for many of their needs.
With technology constantly improving and evolving, people tend to take advantage of the convenience of shopping online. Whether it’s clothing, electronics, or even food, you can easily find almost everything you need on the Internet.
Eyeglasses, unfortunately, are no different. Many online shops have been popping up in recent years, offering people that same convenience. But what...
- Details
- Written by The Community Eyecare Team
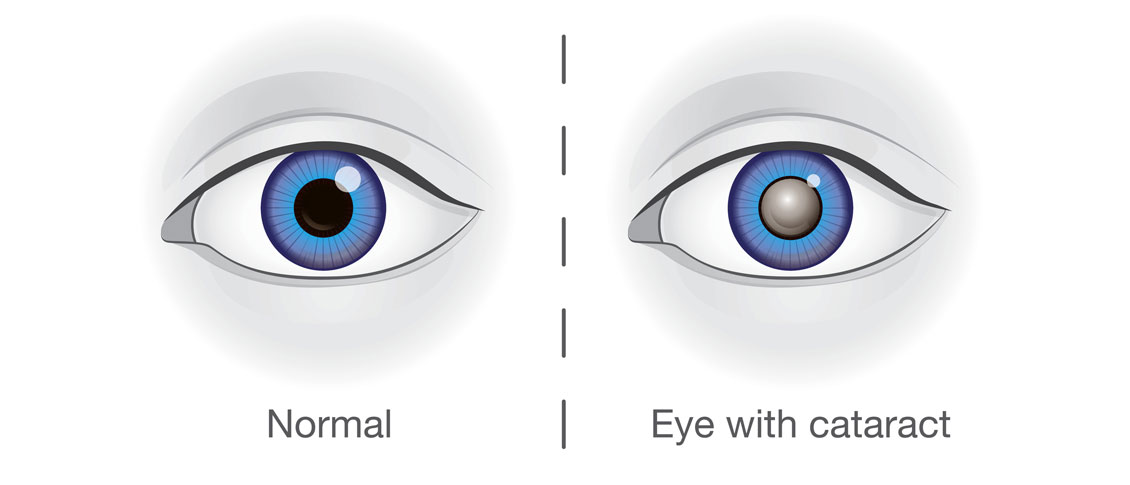
You’ve been diagnosed with a cataract and you’ve been told you should have cataract surgery. The surgeon is also telling you that you should consider paying extra out of pocket it for it.
Where did this come from? Why should you have to pay out of pocket for cataract surgery? Shouldn’t your health insurance just cover it?
In trying to answer those questions, you will first need a little history of both cataract and refractive (correcting errors of refraction such as nearsightedness,...
Patient Resources
Please Leave a Google Review
We sincerely appreciate our patients and welcome your feedback. Please take a moment to let us know how your experience has been.
Our Dry Eye Center
Northeast Wisconsin's Optometrists of Choice
Menasha Office
1255 Appleton Road
Menasha, WI 54952-1501
Phone: (920) 722-6872
CALL 1ST - NO WALK-INS
Brillion Office
950 West Ryan Street
Brillion, WI 54110-1042
Phone: (920) 756-2020
CALL 1ST - NO WALK-INS
Black Creek Office
413 South Main Street
Black Creek, WI 54106-9501
Phone: (920) 984-3937
CALL 1ST - NO WALK-INS
© Community Eyecare, Inc.: 3 Convenient Northeast Wisconsin Locations | Menasha, WI | Brillion, WI | Black Creek, WI | Site Map
Text and photos provided are the property of EyeMotion and cannot be duplicated or moved.